Fever is a prominent feature of the disease since antiquity and even considered as a mighty health engine. Fever is one of the oldest clinical indicators of disease in the mammalian host as well as one of the most common reasons for medical consultations worldwide. Fever is a cardinal response to infection that has been conserved in warm and cold-blooded vertebrates for over 600 million years of evolution. When a child or parent becomes feverish with shivers, chills, and sweats, our first thought is to get the temperature down. Pharmacies sell billions of fever-reducing pills like aspirin and acetaminophen every year, and schools often insist that students stay home until their fever is gone.
But is this “fever phobia” backed up by clinical and scientific findings? Let us find out.
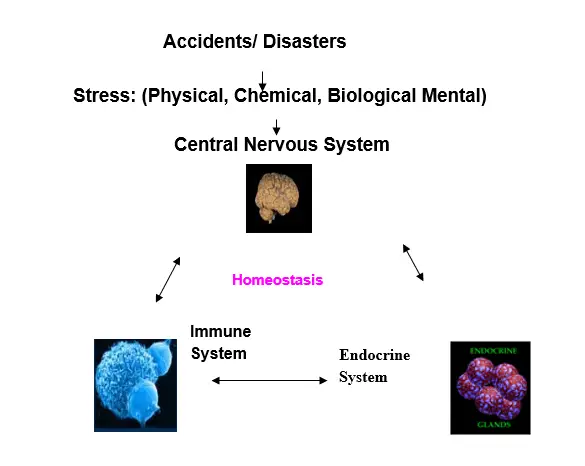
The fever response is orchestrated by the central nervous system through endocrine, neurological, immunological and behavioural mechanisms and confers a survival benefit during infection.( Nat Rev Immunol. 2015:15(6):345, Journal of Infection and Public Health (2011)4, 108). The human body has a thermostat in the hypothalamus that keeps the fever in the optimal range for fighting infections and other insults.
| Normal | 37-38◦C |
| Mild/Low | 38.1-39◦C |
| Moderate grade | 39.1—40◦C |
| High grade | 40.1—41.1.◦C |
| Hyperpyrexia | >41.1◦C |
Definition and Thermoregulation of fever:
Fever is a symptom and not a disease. Fever often occurs in response to infection, inflammation and trauma. A growing body of evidence now suggests that fever represents a complex adaptive response of the host to various challenges whether infectious or non-infectious. The microorganisms which cause infection leading to fever belong mainly to virus, bacteria, parasite and fungi. Further, there are around 200 respiratory viruses known regarding their ability to cause Flu-like Illness. Fever and the febrile response, therefore, remain significant contributors to the pathogenesis, clinical presentation and outcome of hundreds of illnesses and diseases. In healthy individuals, body temperature varies in relation to several environmental and biological factors such as time of day, site of temperature measurements, level of physical activity, age, sex and race, among others. The table above gives the temperature range of various grade fevers (Fever in handbook of signs & symptoms . 3rdedition Lippincott Williams & Wilkins; 2006). In the geriatric group (>65 years), who are likely to have lower body temperatures, Infectious Disease Society of America defines fever as an increase in temperature of >2 ◦F (>1.1 ◦C) over the baseline temperature. Fevers can be classified into acute, sub-acute and chronic fevers based on duration. Acute fevers (<7 days in duration) are characteristics of infectious diseases such as malaria and viral-related upper respiratory tract infection while sub-acute fevers (usually not more than 2 weeks in duration) may be seen in cases of typhoid fever and intra-abdominal abscess, among others. Chronic or persistent fevers (>2 weeks duration) are typical of chronic viral, bacterial infections, cancers and connective tissue diseases.
Fever and survival:
The significance of fever in response to bacterial infection has been investigated using the lizard as an animal model. An elevation in temperature following experimental bacterial infection results in a significant increase in host survival. Was that a design flaw? Why would our bodies waste energy on something that isn’t helpful?
Every aspect of our immune system works better at a higher temperature. A higher temperature in the body speeds up the functioning of cells, including the ones that fight illness. They can respond to invading germs faster. Also, higher body temperatures make it harder for bacteria and viruses to thrive in the body. Dogs, rabbits, mice, ferrets, lizards, fish, and other species when injected with germs had a higher death rate when their fever was suppressed. Humans should be no different. Articles on rhinovirus, influenza, chickenpox, and other respiratory infections all showed improved outcomes if the associated fever was not treated. (Science1975, 188(4184):166, Pediatrics. 1992:90(6):846, N Engl J Med. 1981:305(14):808).
Stress contributes to Infection and Illness:
We have long known that emotions can affect health. Depression, anxiety, stress, all these have an effect on health. There are 2,409 references on how emotions affect the immune system in Pub Med, which is a leading database for medical research (Arch Otolaryngol Rhinol 4(1): 027). The host response to any kind of stress is orchestrated by the three pillars of the disaster management of the body: the brain, endocrine system and the immune system, which talk to each other in bringing the host back to normalcy (see figure).
Psychoneuroimmunology is an interdisciplinary field concerned with the study of behaviour-neuroendocrine-immune interactions and their potential health consequences (Clinical Microbiol Review, 7:200, 1994). Stress has long been identified as a cofactor in the reactivation of the latent virus in humans. Stress was associated with increased nasal secretions following inoculation with rhinovirus or influenza A virus in humans.
Isolation stress (like Quarantine) induced the neuroinvasiveness of Sindbis virus. Stress-induced neuroinvasiveness of a neurovirulent non-invasive Sindbis virus in cold or isolation subjected mice (Life Sci. 48:1493,1991). Stress was associated with an increased infection rate following Coronavirus, Rhinovirus, respiratory or syncytial virus challenge (N. Engl. J. Med. 325:606, 1991).
Fever Measurement:
The core temperature measurement is more reflective of the body temperature. The peripheral temperature measurements on the forehead, wrist, and axillary (armpit) region do not have clinically acceptable accuracy and should not be used, as it may influence clinical decisions (Ann Intern Med 163:768, 2015.). Doctors from Royal Children’s Hospital Melbourne observed that forehead thermometers appear to be the least reliable device at predicting both subsequent fever in hospital and the presence of invasive infection. Considering a) forehead temperature measurement is least reliable b) more than 85% Covid positives ( please read Immunotherapy by Nature vs. Vaccine) are with insignificant disease symptoms c) there are hundreds of reasons to get fevers, relying only on forehead temperature measurement and labelling people as COVID-19 suspect, is beyond the understanding of medical science (Please see Covid-19 lockdown: India’s poor are the hardest hit).
Fever treatment:
Most infectious causes of fever are naturally self-limited (such as viral diseases) or easily treatable bacterial diseases of the pharynx, ears, sinuses, upper respiratory airways, skin, and urinary tract. These illnesses of less than 7 to 10 days do not require hospitalization and result in no long-term effects.
Research has shown that people with infections who are treated with fever-reducing medicines have symptoms that often are more severe and last longer than those who don’t take anti-fever medicines (J Infect Dis. 1990:162(6):1277-1282). Paracetamol is a commonly used, moderately effective analgesic and antipyretic. In overdose, it causes significant morbidity and mortality. (QJM: An International Journal of Medicine, Volume 95: 609, 2002). In a meta‐analysis of two trials, the proportion of children without fever by the second hour after treatment did not differ significantly between those given paracetamol and those sponged. (DOI:10.1002/14651858.CD003676). The use of antipyretic drugs to diminish fever correlates with a 5% increase in mortality in human populations infected with influenza virus and negatively affects patient outcomes in the intensive care unit. To date, there is no published research that shows treating fevers with antipyretics improve outcomes. What about fever from vaccines? Antipyretics cause a lower antibody response when measured one month after vaccination (Lancet. 2009:374(9698):1339). In summary, there is evidence that fever improves outcomes for infections, but there is no evidence to the contrary. Let’s be evidence-based.
It is important to keep patients well hydrated so that they can easily give off heat by sweating. November 1891 issue of the Journal of American Medical Association has written about the importance of diet in fever. The craving of febrile patients for citrus food has been stressed in the paper. Reducing fevers may make you feel better but at the cost of delayed recovery. Many vitamins and trace elements have been shown to be beneficial in controlling infection and regulating fever. Nutrition has been demonstrated to contribute to the host immunity leading to the control of infection (Please read Immunotherapy by Nature Vs Vaccine).
However, fever is not without its ill-effects, especially in cases of very high-grade fevers, or when a high fever is associated with co-morbidities such as severe sepsis, and pre-existing cardiopulmonary disease.

A very good analysis about the fever. Fever is a symptom and not a disease. Forehead temperature measurement is least reliable and that is being used for screening. 38 C is declared as high and persons are sent home or for Civid testing !! What a ridiculous decision!!
Great article Dr Poduval. You have nailed it rightly…feverphobia…has become a good time business in consumer healthcare.
Great insight Dr Poduval. You nailed it rightly… Feverphobia…a great business in consumer healthcare
This information is very vital,who are scared about the pandemic like covid. Since the Fever clinic is maintaining the forehead temp. It is useful for a common man.